Type to search
{{ site.specific_data.Twitter }}
Under Obama, Government’s Safety Net Has Expanded
January 19, 2016
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — Despite Republican majorities in Congress through much of his tenure and increasingly insistent calls from GOP presidential candidates to rein in “free stuff,” President Barack Obama has engineered the largest expansion of the federal government’s safety net in half a century, a record he cemented further as he closed out his seventh year.
The growth of social welfare programs, including health insurance — though sometimes overshadowed by immigration and other partisan issues — is shaping up to be a central issue in the campaign to succeed Obama. Republican presidential hopefuls have called for rolling back much of what Obama has done, while Hillary Clinton and the other Democrats want to go further.
The latest expansions came in the $1.8 trillion budget deal that Congress approved last month, which made permanent hundreds of billions of dollars in tax breaks for low- and moderate-income families and boosted aid for college students.
The tax credits have received much less public attention than other social-welfare spending, including the Affordable Care Act, but they have become the government’s largest cash-assistance program to fight poverty, with more than 40 million people receiving benefits each year.
The assistance was broadened on a temporary basis, mostly in Obama’s first year. Making that expansion permanent will help at least 16 million people, according to estimates from the Center on Budget and Policy Priorities, a left-leaning Washington think tank.
That “would rank among the biggest anti-poverty achievements, outside of health reform, in years,” said Robert Greenstein, the center’s executive director.
The expanded aid for low-income Americans reflects Obama’s belief in leveraging government power to combat income inequality, which he has called “the defining challenge of our time.” Even with the expanded aid, the U.S. tax system provides far more benefits to wealthy Americans than it does to the poor, a point frequently cited by liberals.
Obama’s ability to lock in and even expand his social programs despite Republican congressional majorities has fueled a fury among conservative voters that many direct against the GOP leadership, whom they accuse of repeatedly surrendering to the White House.
After the budget deal, House Speaker Paul Ryan, R-Wis., was forced to defend himself against such critics. “We fought for as much as we could get,” he said on NBC’s Meet the Press. “We’re going to pick up next year … and keep going for more.”
Congressional Republicans’ 2016 budget blueprint — which provides an outline of the party’s governing vision — proposes hundreds of billions of dollars in cuts to Medicaid, food assistance and other programs for the poor.
Many Republican politicians argue that costly government programs such as those Obama has pushed are stunting economic growth, depressing wages and creating a “culture of dependency.”
That argument has proved extremely potent, helping deliver historic GOP majorities in Congress and animating the campaigns of many of the 2016 GOP presidential contenders.
But Republicans have been unable to use their majorities to reverse the growth in social programs, as the year-end budget deal underscored.
In addition to the tax benefits for low-income families, the deal, which gained support from majorities of Democrats and Republicans, also boosted federal aid for low- and middle-income college students through increased grants and tax breaks.
Moreover, it protected the core of the president’s signature Affordable Care Act, although it delayed three taxes included in the law.
“That seems like a pretty worthwhile trade-off,” said former Senate Majority Leader Tom Daschle, D-S.D., a onetime mentor who helped Obama chart his health care agenda after he was first elected.
The 2010 health care law has extended government-subsidized health coverage to millions of poor and working-class Americans in the last two years.
To many Republicans, the failure to repeal it marks the most notable lapse by the GOP leadership. Today, as the law’s coverage expansion enters its third year, close to 20 million low- and moderate-income Americans rely on health insurance provided through the law, including state Medicaid programs for the poor and subsidized commercial insurance available on HealthCare.gov and other government-run insurance marketplaces.
That expansion has driven a historic decline in the nation’s uninsured rate, dropping the share of adults without insurance from 18 percent at the end of 2013 to 11.6 percent in the third quarter of this year, according to national surveys from Gallup.
The number could continue to fall as additional conservative states, including Louisiana, South Dakota and Wyoming, look for ways to expand their Medicaid programs in 2016, following the 30 states that already have used the law to broaden coverage.
College students also got a boost, as Congress voted to increase the maximum Pell Grant to $5,915. That is up 25 percent from when Obama took office, though college tuitions continue to skyrocket.
Low- and moderate-income students can qualify for additional assistance through the permanent extension of the American Opportunity Tax Credit, which was also included in the year-end budget deal.
The college tax credit provides up to $2,500 for tuition or other education expenses. It was also scheduled to expire in 2017.
©2016 Tribune Co. Distributed by Tribune Content Agency, LLC.
Photo: U.S. President Barack Obama waves as he boards Air Force One for Nebraska and Louisiana at Joint Base Andrews in Maryland, January 13, 2016. REUTERS/Carlos Barria
How The Debate Over Health Care Is Changing — Just In Time For The 2016 Election
October 11, 2015
By Noam N. Levey, Tribune Washington Bureau
WASHINGTON — With the first contests of the 2016 presidential campaign just months away, the national health care debate is poised to enter a new phase, more focused on consumers’ pocketbooks than on relitigating the 5-year-old Affordable Care Act.
Hillary Rodham Clinton, who is campaigning on a detailed program to crack down on rising drug prices and runaway medical bills, is making a play for the hearts of voters increasingly irritated about what they have to pay for health care.
In the process, Clinton, the front-runner for the Democratic presidential nomination, has issued an implicit challenge to her Republican rivals, who continue to campaign with broadsides against Obamacare but few details about how they would address consumers’ basic health care worries.
“She is talking to people’s wallets … at a time when health care prices are a huge concern,” said Frank Luntz, an influential Republican strategist who helped develop the GOP’s highly successful campaign to tarnish Obamacare even before the law was enacted. “It’s smart.”
Clinton highlighted her health care plans on a two-day swing through Iowa last week. “We have to be really focused on how we fix what we have so it works better for everyone,” she told a crowd in Davenport on Tuesday.
Clinton’s proposals may not resonate with the many Americans leery of more promises from the federal government, especially after President Barack Obama pledged similar relief when he signed the current law in 2010. But the former secretary of State has focused attention on an agenda that, polls suggest, Americans want their elected leaders to take on.
Making high-cost drugs affordable should be the top health care priority for the next president and Congress, said three-quarters of Americans surveyed nationwide this year.
Most Americans polled also wanted their elected leaders to protect them from surprise out-of-network medical charges. They wanted the government to ensure health plans have sufficient networks. And they wanted more information about the prices of doctors’ visits, tests and procedures, according to the poll, done by the nonprofit Kaiser Family Foundation.
By contrast, fewer than half of respondents wanted their elected officials to deal with concerns about the Affordable Care Act. Just a third wanted it fully repealed.
“Health is really a pocketbook issue more than a political issue now,” foundation President Drew Altman said.
The evolution may reflect in part Republicans’ waning repeal campaign.
More than five years after its enactment, the law has survived two major legal challenges and three national elections. And, contrary to opponents’ warnings, it has extended coverage to millions of Americans without destroying the existing employer-based system that most in the U.S. rely on for health insurance.
But another factor is probably driving Americans’ concerns about drug prices and medical costs.
Over the last decade, the average deductible that workers must pay for medical care before their insurance kicks in has more than tripled — from $303 in 2006 to $1,077 today, according to a recent report on employer-provided coverage from the Kaiser Family Foundation and the nonprofit Health Research & Educational Trust.
That is seven times faster than wages have risen in the same period.
At the same time, nearly a third of Americans with private health insurance have received bills in which they were charged more than they had expected, a recent nationwide Consumer Reports survey showed.
In response, Clinton is proposing a series of new restrictions on insurers and drugmakers.
Among other things, she would put a $250 monthly cap on how much consumers could be required to pay out of pocket for medications. She would allow consumers to buy pharmaceuticals abroad, where they are often substantially cheaper.
Clinton also would create a new tax credit that Americans could use to help defray their out-of-pocket medical expenses.
Insurers would be required to cover at least three doctor visits annually that aren’t subject to a deductible.
And doctors who are providing care at a hospital that is in a patient’s network would be prohibited from charging the patient out-of-network prices.
Clinton is also pushing broader policies to clamp down on the pharmaceutical and insurance industries, including restrictions on drug advertising and new federal oversight of insurance rate hikes. She would also allow the federal government to negotiate lower drug prices for Medicare beneficiaries, something that could save billions of dollars but is currently prohibited.
Vermont Sen. Bernie Sanders, an independent challenging Clinton for the Democratic nomination, is proposing his own six-point plan for reducing drug prices, including allowing the federal government to negotiate Medicare drug discounts.
Some experts have dismissed parts of Clinton’s agenda as unrealistic, especially her proposal to require drugmakers to spend more on research.
But this kind of consumer-focused agenda holds great promise for Democrats who’ve been paralyzed by Republicans’ long campaign against the Affordable Care Act, said Celinda Lake, a veteran Democratic strategist. “This is a post-Obamacare message … that has something for the insured, as well as the uninsured,” she said.
In contrast, none of the leading Republican presidential candidates has a health care plan, though Florida Sen. Marco Rubio published a Fox News op-ed in March calling for broad changes to the health care system, including deregulation of insurance markets to lower costs.
The most detailed health care plan in the Republican field was put forward by former Wisconsin Gov. Scott Walker; he dropped out of the race two weeks ago.
Despite the lack of specifics, the GOP’s simple anti-government, anti-Obamacare message still resonates with large swaths of the electorate.
Although huge majorities of Americans complain about drug prices, for example, substantially fewer support government intervention.
In one recent national survey from market research firm YouGov, 86 percent of respondents said drug prices were either “far too high” or “a little too high,” yet only 50 percent said they would support “the federal government controlling the price of prescription drugs.”
(c)2015 Tribune Co. Distributed by Tribune Content Agency, LLC.
File photo via
Diabetes Study Shows Benefits Of Expanded Medicaid Under Obamacare
March 23, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — Low-income patients with diabetes are getting better access to medical care in states that have expanded Medicaid coverage through the Affordable Care Act, suggests a new study that provides one of the first indications of the sweeping law’s health effects.
Residents of other states are at risk of being left behind.
The number of Medicaid patients with newly identified diabetes surged 23 percent in states that expanded their programs, an option provided by the law, but there was virtually no increase in states that declined to expand coverage, researchers found.
“Clearly, the expansion of Medicaid has had a tremendous impact,” said the study’s lead author, Dr. Harvey Kaufman, senior medical director of Quest Diagnostics. “It has helped a lot of people, and frankly helps anyone who pays.”
Early diagnosis makes diabetes easier to treat and lessens the risk of complications.
The study is published in Diabetes Care, the journal of the American Diabetes Association.
The expansion of Medicaid, the 50-year-old government health plan for the poor, is a pillar of the 2010 health care law, which makes billions of dollars of federal aid available to states if they open their Medicaid programs to low-income adults.
Most states historically provided Medicaid coverage only to poor children, mothers, the elderly and disabled.
Despite the new federal dollars, however, 22 states — all led by either Republican governors or legislatures, or both — have turned down the assistance, citing concerns about Medicaid’s effectiveness and cost.
To assess the potential effects of those decisions, Quest Diagnostics, a leading provider of diagnostic services, analyzed its patient database of blood tests to identify Medicaid patients who were diagnosed with diabetes for the first time in 2014, the year that Medicaid expansions began under the health care law.
The researchers compared the number of newly identified diabetics in 2014 with the number of newly identified diabetics in 2013.
Not only did researchers find more newly identified diabetics in states that expanded Medicaid, they also discovered that the patients were probably being diagnosed earlier.
Newly identified diabetics in Medicaid expansion states had lower hemoglobin A1c levels, a common measure of blood sugar used to assess the progress of the disease, the study found.
Early diagnosis can be crucial for diabetics, said Dr. Robert Ratner, chief scientific and medical officer at the American Diabetes Association.
“We know from a variety of different studies that if you initiate therapy early, diabetes is easier to treat and you can stabilize the disease,” he said. That can head off more serious and costly medical complications later, such as blindness, kidney failure and cardiovascular disease.
Quest has not taken an official position on expanding Medicaid, but the researchers noted the benefits of the coverage expansion.
“We postulate that these Medicaid patients with newly identified diabetes will experience better management of their disease than if diagnoses had been made later,” they wrote in the paper.
The data also could have important implications for other chronic medical conditions that benefit from better access to medical care, such as high blood pressure and high cholesterol.
The architects of the Affordable Care Act had hoped that expanded access to health insurance, such as Medicaid, would ultimately improve Americans’ health.
A growing body of evidence supports this conclusion, though some critics of the law have continued to question the link between insurance coverage and better health outcomes.
Dr. Georges C. Benjamin, executive director of the American Public Health Association, said it was time to end that debate. “This latest study is a strong health argument against those folks who want to repeal the Affordable Care Act,” he said.
Photo: bodytel via Flickr
Supreme Court Arguments To Begin In Major Challenge To Health Care Law
March 04, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — The U.S. Supreme Court is hearing oral arguments Wednesday morning in the latest legal challenge to the Affordable Care Act, a lawsuit that threatens to strip away federal insurance subsidies from millions of Americans and critically undermine the law’s program for expanding health coverage nationwide.
The challenge – spearheaded by conservative and libertarian activists in Washington – was once considered a legal long shot. The architects of the health law, as well as many legal experts and state officials nationwide, have widely rejected the challengers’ interpretation of the law.
But the outcome of King vs. Burwell, as the case is called, is now in doubt, as four conservative justices on the court have made no secret of their hostility toward the sweeping health law President Barack Obama signed five years ago.
In 2012, these justices fell one vote short of overturning the whole law, when Chief Justice John G. Roberts Jr. joined the four left-leaning members of the court to uphold the law’s requirement that Americans have health insurance.
All eyes will be on Roberts, who came under fierce attack from conservatives three years ago for sparing a law that has animated Republican politics since it was enacted.
The current challenge argues that a strict reading of the statute makes health insurance subsidies available only in a handful states that established their own insurance marketplaces through the law.
Thirty-seven states elected instead to have the federal government fully or partially operate their marketplaces using the HealthCare.gov website.
The marketplaces, a central pillar of the law, allow Americans who don’t get health benefits at work to shop online among plans that must offer basic benefits and cannot turn away customers, even if they’re sick.
Consumers making less than four times the federal poverty level – about $47,000 for a single person or $97,000 for a family of four – qualify for subsidies to offset the cost of their premiums.
Those subsidies are considered essential to the marketplaces because they allow healthy people to buy coverage, offsetting the costs of sick consumers.
If the challengers prevail, an estimated 7 million people could lose access to the insurance aid, likely causing widespread disruptions to insurance markets nationwide.
Arguing for the challengers is Michael A. Carvin, a former Reagan administration lawyer who also represented some of the challengers in the 2012 lawsuit against the Affordable Care Act.
He will face the justices for the first 30 minutes of arguments Wednesday morning.
Carvin will be followed by U.S. Solicitor Gen. Donald Verelli Jr., who will defend the law on behalf of the Obama administration.
Verelli was widely criticized for his performance in the health care case before the court three years ago. But he was ultimately vindicated when the court upheld the law.
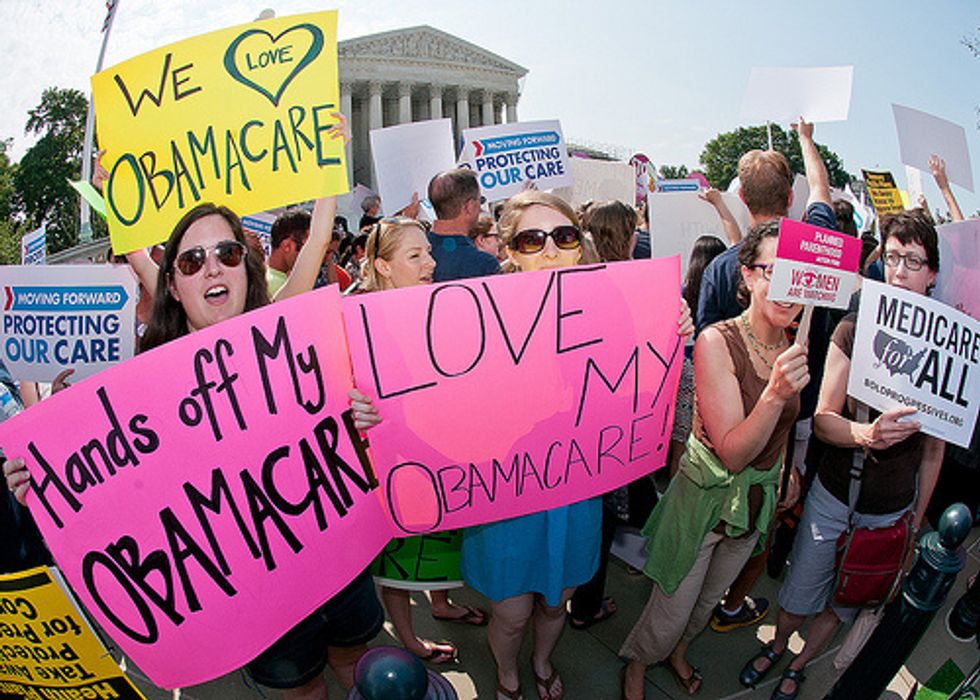
Photo: SEIU International via Flickr
If Supreme Court Rules Against Obamacare, States Have Few Options
March 02, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — With Supreme Court arguments in the latest challenge to the Affordable Care Act just days away, a sense of impending crisis has hit state officials and patient advocates in many parts of the country. Many worry they have no good options.
If the justices rule in favor of the challenge, it would wipe out insurance subsidies for millions of consumers in nearly three dozen states that use the federal HealthCare.gov marketplace established through the health law.
Although consumers could still get aid in states that run their own marketplaces, officials in states that rely on the federal government fear they don’t have the time or resources to set up their own exchanges, even if they could overcome local political opposition.
“The recurrent nightmare for us is … ‘What do we do?’ ” Dr. William J. Hazel, Virginia’s health secretary, said at a recent conference in Washington. “We’re starting from zero. And all of those states like us will probably start at zero.”
The Obama administration, meanwhile, has provided states little guidance, a strategy many believe is calculated to pressure the Supreme Court not to sow chaos by invalidating the aid.
Congressional Republicans also have not advanced alternative plans to help states, though some senior GOP lawmakers say they might restore aid to consumers if the president agrees to change the health law commonly called Obamacare. The deeply divided party hasn’t agreed on what changes to seek, however.
The marketplaces — now in their second year — allow Americans who don’t get health benefits at work to shop online among plans that must all offer basic benefits and cannot turn away customers, even if they are sick.
Americans making less than four times the federal poverty level — or about $94,000 for a family of four — qualify for subsidies to offset the cost of their premiums.
The law’s challengers argue that a strict reading of the statute makes those subsidies available only in states that established their own marketplaces, rather than having the federal government operate the marketplace for them.
The Obama administration, the law’s congressional architects and many outside legal experts disagree.
The justices are likely to decide the case in late spring. If they rule against the administration, nearly 90 percent of health plan enrollees in 34 federal marketplace states — an estimated 7 million people — would lose aid.
To restore it, a state such as Virginia could conceivably set up its own marketplace.
Virginia Governor Terry McAuliffe, a Democrat, has repeatedly supported expanding coverage, calling it a “key component of building a stronger Virginia economy.” About 400,000 Virginians have health plans through HealthCare.gov.
Several other governors, including a few Republicans, have indicated they don’t want to let hundreds of thousands of their residents lose coverage.
“If the court rules, and we find half a million Ohioans without insurance, it’s something we’re going to have to deal with,” Republican Governor John Kasich of Ohio said recently.
Building a state marketplace isn’t likely to be easy, however, especially if the Supreme Court rules in June that subsidies must be terminated immediately.
The Health and Human Services Department operates a complex online system for states through HealthCare.gov. The federal agency staffs call centers with thousands of workers. And in some states, federal officials are regulating health plans, traditionally a state job.
States that set up their own marketplaces spent years preparing for the job at a cost of almost $4 billion in federal aid.
California, whose Covered California marketplace is considered one of the most successful, spent more than $1 billion, according to federal data. Kentucky, which prided itself on operating one of the leaner marketplaces, spent more than $250 million.
The federal grants that helped those states are no longer available, however.
“That money will be gone,” said Hazel, the Virginia health secretary. “So I think we’re going to be looking for private funding, foundation funding. We will probably go back to the administration and beg again, to try to ensure that we can at least keep the folks enrolled.”
Hazel won’t get much help from the state’s Republican-controlled Legislature.
Dr. John O’Bannon, a Republican legislator who chairs a health subcommittee in the Virginia House of Delegates, said lawmakers had no interest in setting up a costly state marketplace.
“The bottom line is that this is a federal problem,” he said. “If the law is upended by the federal courts, the federal government is going to have to fix it.”
Republican resistance would probably be an issue nearly everywhere.
Of the 37 states that rely on HealthCare.gov, only Delaware and Oregon have a Democratic governor and a Democratic legislature.
In some places, such as Missouri, state law explicitly prohibits state employees from implementing the Affordable Care Act.
Oregon and two other states, Nevada and New Mexico, have technically established their own marketplaces but use HealthCare.gov, which probably protects their residents’ access to subsidies.
The widespread Republican opposition and technical barriers to establishing a state marketplace have some supporters of the health law hoping the Obama administration will unilaterally enact a fix.
The administration might, for example, issue regulations that make it easier for states that are already cooperating with the federal government to become state-based marketplaces, even though they would continue to rely on the federal HealthCare.gov site.
Seven states, including Illinois, are currently “partnership” states that provide consumer assistance to residents shopping for health coverage. Another seven help oversee the health plans being sold on HealthCare.gov in their states.
But simply using a federal regulation to label these “state marketplaces” when state leaders have not affirmatively indicated that they want to operate their own marketplace would almost certainly provoke a backlash from opponents of the law.
Last week, Health and Human Services Secretary Sylvia Mathews Burwell warned members of Congress that the Obama administration’s options would be limited.
“We know of no administrative actions that could, and therefore we have no plans that would, undo the massive damage to our health care system that would be caused by an adverse decision,” she said.
___
Wes Venteicher in Chicago contributed to this report.
Photo: ProgressOhio via Flickr
Health Law Drives Down U.S. Rate Of Uninsured Patients, Survey Finds
February 24, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — America’s uninsured rate plummeted last year, with the improvement driven by states that have fully implemented the Affordable Care Act, a new nationwide Gallup survey indicates.
Led by Arkansas and Kentucky, which both saw double-digit declines, seven states saw the percentage of adults without insurance fall by more than 5 percentage points between 2013 and 2014.
All but one of the 11 states with the biggest drops implemented both pillars of the federal health law: expanding Medicaid coverage to low-income adults and setting up a fully or partially functioning state-based marketplace.
“While a majority of Americans continue to disapprove of the Affordable Care Act, it has clearly had an impact in reducing the uninsured rate in the U.S., which declined to its lowest point in seven years in 2014,” Gallup’s Dan Witters wrote in a report outlining the new findings.
While some critics of the health law continue to question its impact on coverage, a growing number of independent surveys show the number of Americans without health insurance fell dramatically last year. The rate had been increasing in the years before the new law went into effect.
Gallup’s poll is among the largest surveys on the issue, with more than 175,000 interviews annually. It found that nationwide the rate of uninsured adults declined from 17.3 percent in 2013 to 13.8 percent last year.
The lowest uninsured rates continue to be primarily in the Northeast and upper Midwest. Massachusetts, whose 2006 coverage expansion became the model for the national law, had the lowest rate at 4.6 percent.
The highest uninsured rates are in the South and West. For the seventh consecutive year, Texas has the worst rate in the country, with nearly a quarter of its adults uncovered.
Gallup’s survey also underscored how the health law may be widening the nation’s health care divide.
States that have fully implemented the law saw a 4.8 percentage point improvement in the share of the adult population with insurance between 2013 and 2014. That was nearly twice the rate of decline in states that have not fully implemented the law.
California, which historically had among the highest uninsured rates, recorded one of the fastest declines. The share of adults without coverage in the state fell from 21.6 percent to 15.3 percent.
Even Connecticut and Maryland, which already had among the highest rates of coverage, saw major declines in the rate of uninsured adults. Connecticut’s rate dropped from 12.3 percent to 6 percent; Maryland’s went from 12.9 percent to 7.8 percent.
All three states have enthusiastically embraced the health law.
By contrast, Texas, where opposition to the health law has been fierce, recorded a decline of less than 3 points, from 27 percent to 24.4 percent.
The Gallup survey results were based on interviews nationwide with 178,072 adults in 2013 and 176,702 adults in 2014. The margin of error is plus or minus 1 or 2 percentage points in most states, though it is closer to 4 percentage points in small states.
Photo: SEIU International via Flickr
Fewer Americans Delay Needed Medical Care In 2014, Survey Says
January 15, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — The number of Americans who put off needed medical care fell substantially last year, according to a new survey that provides one of the fullest pictures to date of how the federal health law may be improving not only insurance coverage but also access to health care.
From 2012 to 2014, the share of consumers delaying a recommended test or treatment or not filling a prescription fell by nearly a third. And the percentage who reported problems with medical bills fell by almost a quarter.
Those are the first declines ever recorded by the biennial national survey by the nonprofit Commonwealth Fund, which began asking Americans about the affordability of medical care a decade ago.
“These declines are remarkable and unprecedented in the survey’s history,” said Sara Collins, the study’s lead author. “They indicate that the Affordable Care Act is beginning to help people afford the health care they need.”
The rise in reported access to care parallels a major expansion in health insurance coverage that began in 2014 through the health law often called Obamacare.
The law offers most Americans who don’t get coverage through an employer the chance to buy a health plan on a new state-based marketplace where insurers must meet basic standards and cannot turn away customers. Low- and moderate-income consumers can get subsidies to offset the cost of their premiums.
In about half the states, very poor Americans can get government Medicaid coverage, largely for free. The remaining states have declined federal aid to expand their Medicaid programs.
National surveys indicate the new coverage options cut the number of uninsured Americans by about 10 million, the largest such decline in half a century.
Some consumers who got health plans through the previous system that allowed insurers to deny coverage to sick customers have seen rates go up.
But the new Commonwealth survey indicates that the new insurance options are probably lightening the health care burden on millions of others. From 2012 to 2014, the percentage of Americans who did not visit a doctor or clinic despite having a medical problem in the previous 12 months fell to 23 percent from 29 percent.
The percentage who did not fill a prescription fell to 19 percent from 27 percent. And the percentage who did not get needed specialist care declined to 13 percent from 20 percent.
There were similar declines in stress from paying for health care; the share of Americans who reported problems paying medical bills in the previous 12 months dropped to 23 percent from 30 percent.
“Declines in medical bill problems nationwide are likely driven by expanded access to health insurance,” the authors concluded.
Despite the gains, the Commonwealth study shows substantial problems with access and affordability persist in the U.S. health care system.
These are particularly acute among low-income Americans. The survey found that even if they had health insurance, a third of adults with incomes below twice the federal poverty level reported problems paying medical bills or were paying off medical debt last year.
Americans living in states that did not expand their Medicaid problems through the federal health law also reported more problems accessing medical care and paying for it, the survey found.
And Collins cautioned that the gains may be jeopardized as more Americans face very high deductibles, a common feature of a growing number of employer health plans and those being sold on marketplaces created by the health law.
The average employee deductible increased 47 percent from 2009 to 2014, according to the most recent annual health benefit survey by the Kaiser Family Foundation and Health Research & Educational Trust.
The Commonwealth survey, based on a random, nationally representative sample of 6,027 adults age 19 and older, was conducted from July to December of last year. It has an overall margin of sampling error of plus or minus two percentage points.
AFP Photo/Karen Bleier
Obamacare’s Guaranteed Health Coverage Changes Many Lives In First Year
January 07, 2015
By Noam N. Levey, Tribune Washington Bureau (TNS)
ALEXANDRIA, Va. — Like many working Americans, Lisa Gray thought she had good health insurance.
That was until she was diagnosed with leukemia in mid-2013, and the self-employed businesswoman made a startling discovery: Her health plan didn’t cover the chemotherapy she needed. “I thought I was going to die,” Gray, 62, said recently, recalling her desperate scramble to get lifesaving drugs.
Through a mix of temporary measures, doctors and patient advocates managed to keep Gray stable for a few months.
But it was a new health plan through the Affordable Care Act that Gray credits with saving her life. The plan, which started Jan. 1, 2014, gave her access to the recommended chemotherapy. Her cancer went into remission in the fall.
It’s been one year since the federal law began guaranteeing coverage to most Americans for the first time, even if they are sick.
Some consumers pay more for insurance. Some pay less. Doctors, hospitals and businesses are laboring to keep up with new requirements. And across the country, “Obamacare” remains a polarizing political issue.
For many Americans like Gray — who were stuck in plans that didn’t cover vital services or who couldn’t get insurance because of a pre-existing medical condition — the law has had a personal, even life-changing impact.
“A couple years earlier, I think I would have been done,” Gray said.
Even the law’s supporters concede more must be done to control health care costs and ensure access to care.
But the insurance guarantee — which includes billions of dollars in aid to low- and middle-income Americans — has extended coverage to about 10 million people who previously had no insurance, surveys indicate. That cut the nation’s uninsured rate more than 20 percent last year, the largest drop in half a century.
The law also changed coverage for millions more people who were in plans like Gray’s that capped or excluded benefits, a once-common feature of health insurance that is now banned.
Working out of a trim, white Colonial in suburban Washington, D.C., Gray thought little of these potential changes when President Barack Obama signed the health law in the spring of 2010. She didn’t involve herself in politics. She’d had health insurance for decades.
With a monthly $1,095 premium, the Kaiser Permanente plan that she had gotten through her husband’s employer wasn’t cheap.
But it was her only option. As a breast cancer survivor, Gray probably wouldn’t have been able to find a new plan; insurers in 2013 could still turn away consumers with pre-existing medical conditions.
Gray was focused on her business as a consultant who helped companies put together bids for government contracts.
In her free time, she volunteered with Susan G. Komen, the nation’s largest breast cancer foundation. “I was in give-back mode,” said Gray, who sports a pink ribbon on her car and displays a pink Halloween pumpkin on her front lawn every year.
Then, on the morning of May 20, 2013, Gray skidded off the road driving to her vacation condominium on Maryland’s Eastern Shore. Aside from a few bruises, she was unhurt.
But she had a bigger surprise at the emergency room. A routine blood test showed an unusually high white blood cell count.
Gray had chronic myeloid leukemia, a relatively uncommon form of cancer that starts in the bone marrow and leads to the production of abnormal blood cells.
The disease is now considered highly treatable. Gray’s oncologist at Kaiser prescribed the standard oral chemotherapy, a medication known as Gleevec.
Much relieved, Gray called her pharmacy to pick up the prescription.
There was a pause on the line. The pharmacist asked Gray if she knew the drug would cost $6,809 a month.
“I freaked out,” she recalled. “Why would they even make this drug if people can’t afford it?”
Neither Gray nor her doctor realized her Kaiser plan only covered $1,500 worth of prescription drugs a year, a provision spelled out in small type in Appendix B of her 80-page plan brochure.
Caps on coverage were once routine; most commercial health plans once put some kind of annual or lifetime limit on how much care they covered.
“Patients often didn’t know they had inadequate coverage until they were diagnosed with a catastrophic illness,” said Dr. S. Yousuf Zafar, an oncologist at Duke Cancer Institute who studies how costs affect cancer care.
Gray desperately looked for help.
She earned too much to qualify for most charity programs that drugmakers offer. Kaiser wouldn’t lift her drug cap. And with a cancer diagnosis, she wouldn’t be able to get a new insurance plan.
At one point, she emailed her sister, a former radiation oncologist, to ask about life expectancy for her without cancer treatment.
“It’s not an option,” her sister, Cecily Bullock, wrote back.
Gray’s family explored going to Canada, where pharmaceuticals are often less expensive. They finally found a clinical trial closer to home at the University of Maryland, Baltimore, where researchers were testing an alternative to Gleevec called ponatinib.
Gray’s cancer quickly responded. The relief was only temporary, however. In late July, she was hospitalized with pancreatitis, a potentially dangerous inflammation of the pancreas.
The next month, Gray had to stop the ponatinib. Without access to either drug, she was again scrambling.
Bristol-Myers Squibb, which provides cancer patients with a temporary insurance card for a 30-day supply of yet another cancer drug, seemed to offer hope. But the card wasn’t accepted at the Kaiser pharmacy where Gray had to get her prescriptions.
American Cancer Society advocate Brandon Costantino, who works with patients at the University of Maryland, Baltimore, persuaded a company sales representative to give Gray a month’s supply anyway.
Then Gray had to contend with yet another obstacle: Patients could typically only get one month of the drug from the manufacturer. She needed a second to keep up treatment through December.
“It was like brick wall after brick wall that we had to chisel through,” said Costantino, who went back to Bristol-Myers Squibb to get the additional chemotherapy. “My mantra for Lisa was: ‘We just need to get you to 2014,'” he said.
Even the promise of a new insurance plan under the Affordable Care Act seemed elusive at first. Gray, like others, battled through the problems that hobbled HealthCare.gov after it opened. “I must have called 85 times or more,” she said.
Finally, on Dec. 2, 2013, she selected a new Kaiser Permanente health plan for $780 a month. That was $315 less than her current plan. Most important, the plan covered Gleevec for a $30-a-month co-pay.
Gray broke down in the pharmacy when she picked up her first prescription last January — she admits she’s “kind of a crier.”
Nine months later, a bone marrow biopsy showed no further sign of leukemia.
Today, Gray is healthy, aside from the occasional sinus infection.
Sitting on her living room couch with her dog, Gray says she is somewhat bewildered by the controversy that continues to shadow the health law.
“I don’t understand why people get so mad. … It’s just health insurance,” she said, describing conversations with friends and neighbors who say the law should be repealed. “I tell them, ‘You have to understand, there are people who need this. I mean really, really need this.'”
Photo: Cancer survivor Lisa Gray poses for a portrait with her dog Riley on Jan. 2, 2015 in her house in Alexandria, Va. Gray was diagnosed with Leukemia in 2013 and the new health plan made available through the Affordable Care Act saved her life. (Olivier Douliery/TNS)
Enrollment For Obamacare Jumps With Two Million New Sign-Ups
December 23, 2014
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — Enrollment in health insurance through the Affordable Care Act is increasing rapidly, with more than two million people so far signing up for coverage for the first time, figures released Tuesday show.
In addition to the new enrollments, which surpass last year’s sign-up rate, several million more people have been re-enrolled in plans in the law’s second year of expanding coverage.
The new tally, outlined in a report from the Department of Health and Human Services, covers the 37 states whose residents can use a federal website to buy coverage. Several hundred thousand additional sign-ups are expected from 13 states, including California, Maryland and Connecticut, and the District of Columbia that run their own online marketplaces.
The numbers provide an early snapshot of how well the law, also known as Obamacare, will work in 2015. They underscore improvement in how the enrollment process is working this year compared with last, when technology problems made sign-ups on Health.Care.gov virtually impossible for consumers for weeks.
Health and Human Services Secretary Sylvia Mathews Burwell called this year’s early tally “an encouraging start.”
“People shopped for coverage and signed up, finding more choices and greater competition,” she said.
The law allows Americans who don’t get health benefits at work to shop among plans on new marketplaces operated by the federal government or by individual states.
Consumers making less than four times the federal poverty level — or about $94,000 a year for a family of four — qualify for subsidies.
This year, consumers who already have coverage through the marketplace had until Dec. 15 to go back and shop for plans before they were automatically re-enrolled in their current plan.
Open enrollment continues through Feb. 15, and those who have automatically been re-enrolled can change to a new plan until then.
According to the report, between Nov. 15 and Dec. 19, nearly 6.4 million people selected health plans or were re-enrolled into plans through Health.Care.gov.
About 1.9 million of those consumers did not previously have a plan through the federal website. The remainder re-enrolled. Most them were automatically moved into a 2015 plan, but Burwell said that more than a third had chosen a new plan on their own, a key step that allows consumers to find the lowest-priced option.
Though complete data from states that run their own marketplaces are not yet available, in California, nearly 100,000 people selected plans by Dec. 11, before the process of automatically re-enrolling current plan holders began.
Total enrollment in the marketplaces, although an imprecise measurement, has been watched closely because sustained growth is considered vital to reducing the number of uninsured and keeping premiums in check by getting healthier Americans into the market.
This fall, the Obama administration substantially reduced enrollment targets for 2015, predicting that 9 million to 9.9 million people probably would get coverage by the end of next year. Currently, enrollment trends appear to be on track to outpace that prediction.
The nonpartisan Congressional Budget Office, which lawmakers rely on to estimate the effect of federal legislation, had predicted that enrollment would hit 13 million customers in the second year of the marketplaces.
About 6.7 million people had health plans through either federal- or state-run marketplaces before the open enrollment period began Nov. 15, according to the Health and Human Services Department.
Overall, surveys suggest that about 10 million uninsured people have gained coverage this year since the marketplaces opened and Medicaid was expanded in many states under the law.
That marks the largest expansion of health insurance coverage in at least half a century and has contributed to a sharp drop in the percentage of working-age Americans who lack insurance. Still, about 30 million people remain uninsured.
AFP Photo/Joe Raedle
Obamacare Adviser Apologizes To Lawmakers For Controversial Comments: ‘I Behaved Badly’
December 09, 2014
By Noam N. Levey, Tribune Washington Bureau (TNS)
WASHINGTON — Jonathan Gruber, an MIT professor who worked on the Affordable Care Act, apologized to members of Congress on Tuesday for a series of controversial comments he made about the law, which Republicans have seized on to attack the health care legislation.
“I behaved badly, and I will have to live with that,” Gruber told the House Committee on Oversight and Government Reform. “But my own inexcusable arrogance is not a flaw in the Affordable Care Act. The ACA is a milestone accomplishment for our nation that already has provided millions of Americans with health insurance.”
Gruber, an economist who advised the White House during the development of the law in 2009 and 2010, was captured in a series of videos speaking disparagingly about voters and the development of the measure.
In one video, he said passage of the law was only possible because of the “stupidity” of the American voter.
In another, he suggested that residents of states that rely on the federal government to operate insurance marketplaces are not eligible for tax subsidies, a key tool in the law that allows millions of Americans to buy health coverage on these marketplaces.
The comments have become a cause celebre for Republicans, who have labeled Gruber an architect of the law, a characterization he disputed Tuesday.
Gruber’s comments have also given ammunition to a legal challenge to the tax credits.
There is widespread agreement among the law’s architects that it allows all low- and moderate-income Americans to receive the tax credits whether they live in states that are operating their own insurance marketplace or live in states that rely on the federal government’s.
But critics assert that language in the law suggests the credits should be limited to state-run marketplaces. The Supreme Court is now considering a lawsuit that could take away credits from millions of Americans in states that do not operate their own marketplaces.
Gruber said Tuesday he does not believe that the credits should be limited.
“I have a long-standing and well-documented belief that health care reform legislation in general, and the ACA in particular, must include mechanisms for residents in all states to obtain tax credits,” he said, noting that the economic models he developed assumed these credits would be available everywhere.
Gruber also noted that contrary to his earlier statements, the law was not developed secretly. “Reasonable people can disagree about the merits of these policies, but it is completely clear that these issues were debated thoroughly during the drafting and passage of the ACA,” he said.
Committee Chairman Darrell Issa (R-A) and other Republicans nevertheless kept up their attacks on Gruber for what Issa termed “arrogance and deceptions surrounding the passage and implementation of Obamacare.”
AFP Photo/Joe Raedle
In Arizona, Swings In Medicaid Access Show Program’s Impact
December 02, 2014
By Noam N. Levey, Tribune Washington Bureau (TNS)
TUCSON, Ariz. — Bad timing turned Karen Slone’s medical problem into a crisis.
Slone, 53, a former administrative assistant with diabetes, followed doctors’ advice for years, getting regular checkups. Then, last year, she lost her job and her insurance, and stopped going to the doctor.
When she spotted a sore on her foot, a common complication of diabetes, Slone tried Neosporin and Band-Aids. By the time she went to an emergency room weeks later, she had a raging infection. Surgeons had to remove bones in two toes.
“It was awful,” Slone recalled. “If I’d have been covered, I would have gone to the doctor sooner.”
For low-income adults like Slone, Arizona was once a trailblazer in health care, providing broad access to Medicaid, the government health plan for the poor.
But during the last recession, Arizona cut coverage for tens of thousands of people. This year, the state expanded Medicaid again, although the decision faces a legal challenge.
Arizona’s on-again, off-again approach makes it a useful place to look at the impact of a program that covers more than one in five Americans.
In 27 states, low-income adults are guaranteed Medicaid coverage through the Affordable Care Act, which provides billions of federal dollars to states to expand the program.
Poor adults are largely shut out of coverage in the remaining states, mostly in the South and interior West. These states declined federal aid, citing concerns about Medicaid’s effectiveness and cost.
Around Tucson’s high desert valley, the effects of Arizona’s shifts in insurance have shown up in breast clinics and emergency rooms, operating theaters and jails.
The changes have affected how sick people became, and even how long they lived, researchers found.
“We’ve gotten to live through a good Medicaid program and a bad Medicaid program,” said Judy Rich, a former nurse who heads Tucson Medical Center. “It made a difference.”
Arizona was the last state to join Medicaid, setting up a program in 1982, nearly two decades after President Lyndon B. Johnson signed the law that offered federal aid to states to insure poor families and the disabled.
The program initially provided more limited benefits than most states. But in the late ’90s, Arizona took an unexpected turn.
Pushed by doctors, civic leaders and hospitals — many from the more liberal Tucson area — voters approved ballot measures to dramatically expand Medicaid, paying for it with Arizona’s share of a legal settlement between states and the tobacco industry.
In most states at the time, Medicaid was reserved primarily for poor children, mothers and the disabled. Arizona joined a handful offering coverage to low-income working-age adults, even if they didn’t have children.
The vote fueled the fastest Medicaid expansion in the country: Enrollment more than doubled between 2001 and 2010 to 1.3 million people.
In Tucson, that spawned new clinics and programs for the needy. It also appears to have improved residents’ health.
Mortality rates in Arizona, New York and Maine, which all expanded Medicaid between 2001 and 2003, fell 6 percent compared with neighboring states that did not expand, researchers found.
The decline was most pronounced in places with large poor populations such as Tucson and surrounding Pima County, where Medicaid probably had the biggest effect, according to the study in the New England Journal of Medicine.
“The expansion was very effective,” said Neal Cash, president of Community Partnership of Southern Arizona in Tucson, which manages behavioral health services for more than 200,000 poor patients. “Before, people were literally being treated in the streets.”
When tax revenues plunged during the 2008-09 recession, however, Arizona froze Medicaid enrollment for childless adults and dropped services. The retrenchment was one of the most severe in the country.
Doctors and others quickly noticed changes.
At Dr. J. Manuel Arreguin’s gynecology clinic on the lower-income south side of Tucson, women began delaying recommended surgery for fibroids, noncancerous growths that appear in the uterus and can cause serious bleeding.
Pima County jail officials noticed that more inmates needed extra medical attention, even kidney dialysis. Many had lost health insurance and access to medications and medical services before they were arrested.
In rural health clinics, patients started drifting away; many sought care or drugs in Mexico, said Amanda Aguirre, president of the Regional Center for Border Health.
And at Tucson Medical Center, doctors and nurses struggled to get patients to seek follow-up care.
“It seemed like all of a sudden, half the people didn’t have health coverage,” said Dr. Michelle Williams, assistant medical director of the hospital’s emergency department. “I didn’t want to ask about coverage because it is not what I’m supposed to do as a physician. But you had to.
“I’d make a plan for a patient, and then they would say, ‘That’s not going to work because I don’t have insurance.’ ”
Among the Medicaid services the state cut four years ago was podiatry, an important benefit for diabetics, many of whom lose feeling in their feet and become more prone to infections as the disease wastes nerves and arteries.
At the University of Arizona Medical Center in Tucson, Dr. David Armstrong still sees the impact.
Nearly every day, Armstrong and Dr. Joseph L. Mills, who co-direct the Southern Arizona Limb Salvage Alliance, don surgical scrubs and step into an operating room to amputate limbs or cut away diseased bones and flesh of patients with diabetes who put off seeing a doctor.
One afternoon, Armstrong’s team labored to save the black, gangrenous left foot of a 30-year-old diabetic, sawing out infected bones, stitching healthy tissue and grafting skin in a bid to spare him life in a wheelchair.
“If it was just a couple of months earlier, we probably could have stopped some of these problems,” Armstrong said later. “We’re constantly shaking our heads.”
Armstrong and other researchers documented a 37 percent increase in hospital admissions for diabetic foot ulcers between 2006 and 2011, according to a study they published in the journal Diabetes Care.
Patients also stayed longer in the hospital with more severe outcomes, they found. Amputations, surgical complications, life-threatening infections and deaths increased by nearly half.
“These people’s feet were literally killing them,” Armstrong said.
What’s frustrating, he said, is that the solution is straightforward. “It doesn’t need big, fancy machines. … It’s just good, quality primary care.”
Sitting in her living room in a modest apartment complex in Tucson, Slone counts herself lucky that her injury wasn’t worse.
She can walk. And she got a new job at a call center this summer, which soon should give her health insurance again.
She is still struggling with more than $30,000 in medical bills, however, and has had a new flare-up on her foot.
Many other Arizonans have gained coverage since January after Republican Gov. Jan Brewer’s push for Medicaid expansion. Enrollment surged 26 percent this year to more than 1.6 million, state figures show.
Although podiatry services haven’t been restored, the expansion of the safety net is already being felt.
At Tucson Medical Center, the number of life-threatening cases in the emergency room has declined.
Doctors instead are seeing more patients with severe headaches or abdominal pain. The symptoms can indicate a very serious condition, but uninsured patients often ignore them, fearing the high bills they may face.
At the hospital’s breast clinic, the waiting list for screening through the hospital’s charity program, which had been three months, is now half as long.
Officials at the Pima County jail have been busily signing up inmates for Medicaid all year. Capt. India Davis, the assistant corrections director, said officials expect the improved access to health care, especially behavioral health services, will not only lessen the burden on the lockup but also reduce recidivism.
But the state’s swings in policy may not be over.
A group of GOP state lawmakers is suing to roll back the Medicaid expansion.
And Gov.-elect Doug Ducey, a Republican who will succeed Brewer in January, hasn’t specified whether he will maintain the new safety net coverage.
Photo: Foot surgeon Dr. David Armstrong, center with blue cap, removes infected bones from diabetic patient Jesus Duarte on Oct. 27, 2014 at the University of Arizona Medical Center in Tucson, Ariz. Armstrong is a member of Southern Arizona Limb Salvage Alliance and has seen a huge increase in serious foot problems from diabetics since Arizona stopped Medicaid coverage for podiatry exams. “People’s feet are killing them,” he said. (Don Bartletti/Los Angeles Times/TNS)
Obamacare Enrollment Surpasses 500,000 In First Week
November 26, 2014
By Noam N. Levey, Los Angeles Times (TNS)
More than half a million people selected a health insurance plan in the first week of the 2015 e2nrollment period under the Affordable Care Act, a new federal report indicates.
Between Nov. 15 and Nov. 21, the U.S. Department of Health and Human Services reported, 462,125 people signed up for a plan through HealthCare.gov, the federally run insurance marketplace that serves 37 states nationwide.
Tens of thousands of additional people signed for coverage on state-run marketplaces in the remaining 13 states, including California, Maryland and Connecticut, and the District of Columbia.
The HealthCare.gov total — which is split roughly evenly between new enrollees and people renewing coverage they had in 2014 — is a major advance from last year, when the website did not work for more than a month.
This year, it appears that the site is working far better. More than 3.7 million users visited HealthCare.gov in the first week of the new enrollment period, according to the health agency.
And in another indication of improvement, wait times at call centers around the country averaged only a little more than three minutes.
Still, it remains unclear whether the Obama administration will be able to hit enrollment targets by the time the sign-up period closes in two months.
The tally released Wednesday counts only plan selections, not the number of people who have paid premiums, which is usually lower. Consumers have until the middle of December to pay in order to guarantee they have coverage starting Jan. 1.
“We had a solid start, but we have a lot of work to do every day between now and Feb. 15,” Health and Human Services Secretary Sylvia Burwell said in a statement, referring to the date that open enrollment ends.
The law this year allowed Americans who don’t get health benefits at work to shop among plans on new state-based marketplaces.
Consumers making less than four times the federal poverty level — or about $94,000 for a family of four — qualify for subsidies.
Total enrollment in the marketplaces, although an imprecise metric, has been watched closely because sustained growth is considered vital to reducing the number of uninsured and keeping premiums in check by getting healthier Americans into the market.
The Obama administration has already substantially reduced enrollment targets for 2015.
Instead of 13 million customers in the second year of the marketplaces, as had been predicted, the Department of Health and Human Services now says 9 million to 9.9 million people probably will get coverage by the end of next year.
About 6.7 million people had health plans through the marketplaces before the current open enrollment period began Nov. 15, according to the federal agency.
Administration officials last week were forced to downgrade that tally from 7.1 million after it was discovered that the figure included some 400,000 people who had only dental plans.
Surveys suggest that about 8 million to 10 million uninsured people have gained coverage this year since the marketplaces opened and Medicaid was expanded in many states under the law. Some 30 million people remain uninsured, however.
AFP Photo/Joe Raedle
A Strategic Shift On Ebola Care
October 17, 2014
By Noam N. Levey and Michael Muskal, Tribune Washington Bureau (MCT)
WASHINGTON — The federal government effectively began to restrict the care of Ebola patients to hospitals with special bio-containment units Thursday, and the Obama administration labored to reassure jittery Americans and increasingly skeptical lawmakers that public health authorities can prevent a widespread Ebola outbreak here.
The tacit shift in policy came amid growing concerns about mistakes at Texas Health Presbyterian Hospital in Dallas, where two nurses who treated Thomas Eric Duncan of Liberia have since come down with the disease.
One of the nurses is being treated at Emory University Hospital in Atlanta, and the other was being transferred to a specialized treatment center at the National Institutes of Health near Washington.
On Capitol Hill, lawmakers demanded answers from the director of the U.S. Centers for Disease Control and Prevention, Dr. Thomas Frieden, who has acknowledged his agency’s lapses in responding to the disease, including allowing one of the nurses to board a commercial flight after she treated Duncan.
Frieden strenuously defended the CDC’s efforts.
“CDC works 24/7 to protect Americans. There are no shortcuts,” he said. “We have a team of 20 of some of the world’s top disease detectives in Texas now. We were there. We left the first day (Duncan) was diagnosed.”
Despite repeated assurances from Frieden and other top health officials that the risk of a widespread outbreak is extremely low, fear of the deadly disease has led to school closings and a suggested ban on travel from the U.S. to and from West Africa — which President Barack Obama said Thursday evening that he might consider in the future.
Domestic air travel was of more immediate concern in Texas and Ohio, where several public schools closed as a precaution after officials learned that faculty and students had flown on the same plane as Ebola patient Amber Vinson, the second of Duncan’s nurses to be diagnosed with the virus that killed him.
Now hospitalized at Emory, Vinson flew to Cleveland on Friday, returned to Dallas-Fort Worth late Monday and was diagnosed with Ebola on Wednesday.
Eight people who came into contact with Vinson quarantined themselves and are being monitored, according to health officials there.
Officials also are asking anyone who visited an Akron bridal shop that Vinson visited Saturday to contact health officials.
The deadly virus is transmitted by the bodily fluids of a symptomatic person.
In Dallas, where fears about Ebola are highest, local officials signed off on “control orders” Thursday that will restrict those being monitored for Ebola from using public transportation or venturing out to public places such as grocery stores.
Dallas County Judge Clay Jenkins said he expected officials to start serving the orders on 75 health care workers Thursday. During an emergency meeting of county leaders, Jenkins said the addresses of those being monitored would be flagged for first responders but not publicly distributed.
Growing public anxiety has fueled Republican lawmakers’ escalating attacks on the Obama administration.
“People are scared,” House Energy and Commerce Committee chairman Fred Upton, R-Mich., told federal health officials at the Washington hearing. “People’s lives are at stake, and the response so far has been unacceptable.”
GOP lawmakers and some Democrats urged a travel ban on passengers from Liberia, Sierra Leone and Guinea, the three West African countries at the center of the Ebola outbreak.
Many public health experts oppose such a move. And Thursday, Frieden also rejected that call, noting it would likely induce travelers from the heart of the outbreak to go underground.
“Right now, we know who’s coming in,” he said. “If we try to eliminate travel, the possibility that some will travel over land, will come from other places, and we don’t know that they’re coming in, will mean that … when they arrive, we wouldn’t be able to impose quarantine as we now can if they have high-risk contact.”
On Thursday evening, Obama said he might consider imposing a ban on travel to Ebola outbreak areas, but he fears it could encourage the sick to hide their illness and result in “more cases rather than less.” But the president said he “may consider it if experts recommend it.”
Obama emphasized, as have Frieden and others, the need to focus on containing the outbreak in West Africa.
The president signed an executive order Thursday authorizing the Pentagon to call up additional Ready Reserve forces to assist in the ongoing U.S. military effort to combat Ebola in Liberia, Sierra Leone and Guinea.
The order was aimed at calling up personnel with key skills, according to an administration official; so far the Pentagon had identified just eight people for the mission.
Obama also met at the White House for the second day in a row with senior officials coordinating the federal Ebola response.
Administration officials have insisted for months that a wider Ebola outbreak in the U.S. is unlikely because American hospitals can effectively isolate and care for infected patients, a key capacity missing in West Africa.
But the apparent breakdown at Texas Health Presbyterian in Dallas that led to the infection of Duncan’s nurses has prompted growing calls for a new system to concentrate care in designed facilities.
The U.S. has four specialized facilities, including Emory, the NIH in Bethesda, Md., the Nebraska Medical Center in Omaha and St. Patrick’s Hospital in Missoula, Mont.
Officials at Texas Presbyterian have acknowledged that they erred in sending Duncan home when he initially came to the hospital with flu-like symptoms and reported he had recently been in West Africa.
On Thursday, Dr. Daniel Varga, chief clinical officer of Texas Health Resources, which owns the hospital, testified at the congressional hearing that the hospital had not trained the medical staff to deal with Ebola, even after the CDC alerted U.S. hospitals to watch for possible cases.
Nevertheless, Nina Pham, the first nurse to be infected, had remained at Texas Presbyterian since her diagnosis over the weekend.
The hospital said in a statement Thursday that officials decided to transfer her because so many of the hospital’s staff are being monitored for Ebola.
Pham was in good condition, according to health officials.
(Levey of the Tribune Washington Bureau reported from Washington and Muskal of the Los Angeles Times from Los Angeles. Times staff writers Molly Hennessy-Fiske and Geoffrey Mohan in Dallas, Kathleen Hennessey and Christi A. Parsons of the Tribune Washington Bureau in Washington and Christine Mai-Duc of the Times in Los Angeles contributed to this report.)
AFP Photo/Nicholas Kamm
Ebola Patient Nina Pham To Be Relocated; Congress Grills Health Officials
October 16, 2014
By Noam N. Levey, Tribune Washington Bureau (MCT)
WASHINGTON — The first Texas nurse to contract Ebola is being moved to a National Institutes of Health clinic near Washington, health officials said Thursday during a congressional hearing about the breakdowns that led to the spread of the deadly virus in Dallas.
Anthony Fauci, director of the NIH’s National Institute of Allergy and Infectious Diseases, said that Nina Pham’s condition is stable and that she is “doing reasonably well.”
The nurse was diagnosed with Ebola on Sunday after treating Thomas Eric Duncan, the Liberian man who died last week at Texas Health Presbyterian Hospital. Pham is being transferred to the NIH Clinical Center in Bethesda, Md. — which has treated other Ebola patients — so she can be in a state-of-the-art facility, Fauci said.
Meanwhile, in Texas and Ohio, some public schools were closed as a precaution Thursday after officials learned that faculty and students had flown on the same plane as Ebola patient Amber Vinson. Vinson, a nurse who also treated Duncan at Texas Health Presbyterian, flew from Cleveland to Dallas-Fort Worth late Monday and was diagnosed with Ebola on Wednesday.
Belton Independent School District, about 130 miles south of Dallas, closed two elementary schools and a middle school.
“Canceling classes at the three campuses will allow us to thoroughly clean and disinfect the schools and buses that served them this week. It will also allow health officials additional time to reassess the health risk to passengers on the plane,” Belton District Supt. Susan Kincannon said in a statement.
Kincannon said the district was notified late Wednesday that the Centers for Disease Control and Prevention was re-evaluating the health risk to some passengers on Frontier Airlines Flight 1143.
In Ohio, the Solon City School District in the Cleveland suburbs closed an elementary and a middle school, spokeswoman Tamara Strom said.
“Two students from these schools were on the same plane that carried the Ebola patient, but not the same flight,” Strom said. “This is totally precautionary as we try and figure out the health situation.”
In Washington, senior federal health officials and the head of the Dallas hospital where the two nurses contracted Ebola were testifying before House lawmakers Thursday afternoon to try to explain the breakdowns that led to the virus’ spread.
Dr. Daniel Varga, the chief clinical officer of Texas Health Resources, which owns the hospital, plans to apologize for breakdowns in the care of Duncan.
“Unfortunately, in our initial treatment of Mr. Duncan, despite our best intentions and a highly skilled medical team, we made mistakes,” Varga says in his prepared testimony.
“We did not correctly diagnose his symptoms as those of Ebola. We are deeply sorry.”
Varga also is to testify that the hospital is working diligently with federal officials to identify where breakdowns in safety protocols may have occurred, causing two nurses who care for Duncan to also be infected.
The hearing before the House Energy and Commerce Committee’s oversight subcommittee is giving members of Congress their first opportunity to grill federal officials since the Texas health workers were diagnosed with Ebola.
A growing number of Republican lawmakers are calling on the Obama administration to take stronger steps to cut off travel from West Africa and strengthen the federal government’s response to Ebola in the United States.
Dr. Thomas Frieden, head of the federal Centers for Disease Control and Prevention, has sought to reassure lawmakers and the public that the agency is stepping up assistance to local hospitals to prevent further spread of the disease.
And in his prepared testimony, the CDC director again expressed confidence that a wider outbreak in this country was highly unlikely.
“As we learn from the recent importation case in Dallas and subsequent transmissions, and continue the public health response there, we remain confident that Ebola is not a significant public health threat to the United States,” Frieden said.
“It is not transmitted easily, and it does not spread from people who are not ill, and cultural norms that contribute to the spread of the disease in Africa — such as burial customs and inadequate public health measures — are not a factor in the United States. We know Ebola can be stopped with rapid diagnosis, appropriate triage, and meticulous infection-control practices in American hospitals.”
AFP Photo/Nicholas Kamm
Obamacare Enrollment At 7.3 Million In August, Down From April
September 18, 2014
By Noam N. Levey, Tribune Washington Bureau
WASHINGTON — Enrollment in health plans offered through the Affordable Care Act dipped slightly through this year, falling from about 8 million this spring to 7.3 million in mid-August, the Obama administration announced Thursday.
The tally represents the first update the administration has provided since the open enrollment period under the health law closed in April.
It suggests that the vast majority of consumers who signed up for coverage this year stuck with it, contrary to warnings from critics of the law that millions would stop paying their premiums.
Marilyn Tavenner, who as head of the federal Centers for Medicare and Medicaid Services oversees new insurance marketplaces created by the law, expressed satisfaction with the enrollment total. “We are encouraged by the number of consumers who paid their premiums and continue to enroll,” she told a congressional panel.
The decline since April also offers a warning, however.
Because the law’s long-term sustainability depends on millions more people signing up for health coverage in coming years, its supporters will have to reverse the erosion in coverage when the second sign-up period begins this fall.
“The challenge in the coming year will be signing up more people for coverage, especially reaching those who stayed on the sidelines this year,” said Larry Levitt, senior vice president at the nonprofit Kaiser Family Foundation, which has been closely tracking implementation of the law.
The law this year for the first time allowed Americans who don’t get health benefits at work to shop among plans on new marketplaces. Those making less than four times the federal poverty level — or about $94,000 for a family of four — qualify for subsidies.
The marketplaces were open for general enrollment from October into April.
But experts always believed the enrollment total would fluctuate through the year, as was common in the old insurance market.
Consumers who did not sign up initially could still enroll later in the year if they lost a job, got divorced, or had another change in circumstance that entitled them to sign up.
Other consumers were expected to drop out as they got other insurance through a new job or qualified for a government program such as Medicare or Medicaid.
The federal government has also been reviewing consumers’ eligibility through the year and moving to cut coverage for people who may not qualify because they do not meet immigration or other requirements.
Administration officials would not say Thursday how many people have been deemed ineligible. But earlier this week, officials warned that as many as 500,000 people could lose coverage this month or be asked to pay more because they did not provide adequate documentation.
Critics of the law have long suggested that the biggest challenge would be keeping consumers who signed up but didn’t pay.
Over the summer, the CEOs of Aetna and Cigna, two of the nation’s largest insurers, warned investors that the companies were seeing a decline in enrollment through the year.
But many other insurers say privately that their enrollment has held steady through the year or increased slightly.
AFP Photo/Karen Bleier
Interested in national news? Sign up for our daily email newsletter!
Obamacare Subsidies Push Cost Of Health Law Above Projections
June 18, 2014
By Noam N. Levey, Tribune Washington Bureau
WASHINGTON — The large subsidies for health insurance that helped fuel the successful drive to sign up roughly 8 million Americans for coverage under the Affordable Care Act may push the cost of the law considerably above current projections, a new federal report indicates.
Nearly 9 in 10 Americans who bought health coverage on the federal government’s health care marketplaces received government assistance to offset their premiums.
That assistance helped lower premiums for consumers who bought health coverage on the federal marketplaces by 76 percent on average, according to the new report from the Department of Health and Human Services.
Premiums that normally would have cost $346 a month on average instead cost consumers just $82, with the federal government picking up the balance of the bill.
While the generous subsidies helped consumers, they also risk inflating the new health law’s price tag in its first year.
The report suggests that the federal government is on track to spend at least $11 billion on subsidies for consumers who bought health plans on marketplaces run by the federal government, even accounting for the fact that many consumers signed up for coverage in late March and will only receive subsidies for part of the year.
That total does not count the additional cost of providing coverage to millions of additional consumers who bought coverage in states that ran their own marketplaces, including California, Connecticut, Maryland and New York. About a third of the 8 million people who signed up for coverage this year used a state-run marketplace.
Federal officials said subsidy data for these consumers were not available.
If these state consumers received roughly comparable government assistance for their insurance premiums, the total cost of subsidies could top $16.5 billion this year.
That would be far higher than projections this spring from the nonpartisan Congressional Budget Office that the 2014 subsidies would cost the federal government $10 billion. Instead, the number would be more in line with earlier estimates from the budget office, which had been revised downward when analysts believed fewer people would sign up for coverage. In the end, enrollment exceeded expectations.
The state-based marketplaces — a centerpiece of the Affordable Care Act — enable Americans who do not get health coverage at work to select among plans that offer at least a basic set of benefits. The plans cannot turn away sick people.
Consumers who make less than four times the federal poverty level, or about $94,000 for a family of four, qualify for subsidies to offset the cost of their premiums in most places.
Obama administration officials Tuesday focused on the availability of affordable coverage for millions more consumers.
“What we’re finding is the marketplace is working. Consumers have more choices, and they’re paying less for their premiums,” Health and Human Services Secretary Sylvia Burwell said in a statement.
But officials who worked on the report refused to speak on the record or discuss the potential impact of the subsidies on the long-term cost of the health law.
Although the law’s costs have thus far been lower than projected, some experts question whether the subsidies will be sustainable.
The Congressional Budget Office estimated in April that the annual cost of subsidies will rise to $23 billion next year and $95 billion in 2024, although the budget office continued to project that all the law’s costs will be offset by additional revenue it raises and by cuts in other federal healthcare spending.
AFP Photo/Karen Bleier
About The National Memo
The National Memo is a political newsletter and website that combines the spirit of investigative journalism with new technology and ideas. We cover campaigns, elections, the White House, Congress, and the world with a fresh outlook. Our own journalism — as well as our selections of the smartest stories available every day — reflects a clear and strong perspective, without the kind of propaganda, ultra-partisanship and overwrought ideology that burden so much of our political discourse.
TAGS